Page 62 - Robeson Living Spring 2019
P. 62
Gibson Cancer Center welcomes Duke Fellows
J
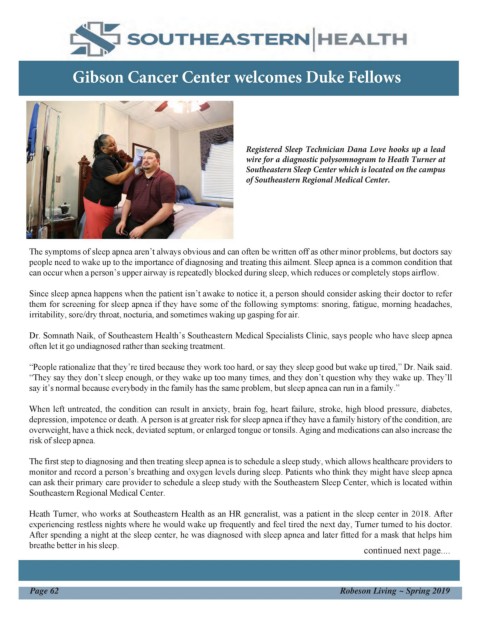
Registered Sleep Technician Dana Love hooks up a lead
wire for a diagnostic polysomnogram to Heath Turner at
Southeastern Sleep Center which is located on the campus
of Southeastern Regional Medical Center.
D
r
. The symptoms of sleep apnea aren’t always obvious and can often be written off as other minor problems, but doctors say
L people need to wake up to the importance of diagnosing and treating this ailment. Sleep apnea is a common condition that
a can occur when a person’s upper airway is repeatedly blocked during sleep, which reduces or completely stops airflow.
u Since sleep apnea happens when the patient isn’t awake to notice it, a person should consider asking their doctor to refer
r them for screening for sleep apnea if they have some of the following symptoms: snoring, fatigue, morning headaches,
a irritability, sore/dry throat, nocturia, and sometimes waking up gasping for air. SR
M M By Roxana Ross
u Dr. Somnath Naik, of Southeastern Health’s Southeastern Medical Specialists Clinic, says people who have sleep apnea
s often let it go undiagnosed rather than seeking treatment. C The field of neonatal
s therapy is relatively
e “People rationalize that they’re tired because they work too hard, or say they sleep good but wake up tired,” Dr. Naik said. NI new, and Southeastern
l “They say they don’t sleep enough, or they wake up too many times, and they don’t question why they wake up. They’ll Health’s Southeastern
w say it’s normal because everybody in the family has the same problem, but sleep apnea can run in a family.” CU Regional Medical
h Center is very proud to
i When left untreated, the condition can result in anxiety, brain fog, heart failure, stroke, high blood pressure, diabetes, off have two therapists
t depression, impotence or death. A person is at greater risk for sleep apnea if they have a family history of the condition, are who can work in the
specialized
highly
overweight, have a thick neck, deviated septum, or enlarged tongue or tonsils. Aging and medications can also increase the
e risk of sleep apnea. ers environment of the
The first step to diagnosing and then treating sleep apnea is to schedule a sleep study, which allows healthcare providers to rar Neonatal Intensive
Care
(NICU).
Unit
monitor and record a person’s breathing and oxygen levels during sleep. Patients who think they might have sleep apnea Since 2016,
can ask their primary care provider to schedule a sleep study with the Southeastern Sleep Center, which is located within e Occupational Therapist
Southeastern Regional Medical Center. and Inpatient Rehab
ne Services Coordinator
Heath Turner, who works at Southeastern Health as an HR generalist, was a patient in the sleep center in 2018. After Jyutika Zope and
experiencing restless nights where he would wake up frequently and feel tired the next day, Turner turned to his doctor. Physical Therapist
After spending a night at the sleep center, he was diagnosed with sleep apnea and later fitted for a mask that helps him on William Hunt have
breathe better in his sleep. continued next page.... been working with
ata full-term and
premature babies at
l SRMC. Their work is
aided
by
upgrades
Page 62 Robeson Living ~ Spring 2019 made in 2017 to the
the unit, which can care
rap for babies born up to
10 weeks early.
work “Not a lot of therapists
in the y go into the NICU,”
highly Hunt said. “It requires
special
ized additional training and
enviro mentorship, it’s and
so
because
nment specialized, it can be
of the hard to find people to
Neona
tal mentor you in this
Intensi area. We conduct
evaluations,
develop
ve treatment plans, and
Care as they gress to go
Unit
(NICU SeHe home, we integrate the
). Since family into that plan.”
2016, alth
Occup
ational anno
Thera
pist unce
and
Inpatie s new
nt
Rehab walk-
Service
s in
Coordi
nator
Jyutika clin
Zope
and
Physic
al
Thera
pist
Willia
m
Hunt
have
been
workin
g with
full-
term
and
premat
ure
babies
at
SRMC.
Their
work is
aided
by
upgrad
es
made
in
2017
to the
unit,
which
can
care
for
babies
born
up to
10
weeks
early.
“Not a
lot of
therapi
sts go
into
the
NICU,
” Hunt
said.
“It
require
s
additio
nal
trainin
g and
mentor
ship,
and
becaus
e it’s so
special
ized, it
can be
hard
to find
people
to
mentor
you in
this
area.
We
conduc
t
evalua
tions,
develo
p
treatm
ent
plans,
and as
they
progre
ss to go
home,
we
integra
te the
family
into
that
plan.”
Kayla
White,
of
Lumbe
rton, is
a nurse
at
SRMC
who is
also a
parent
of a
child
who
went
throug
h the
NICU.
Her
son,
Harris
on,
who
turns 1
this
weeken
d, was
born
six
weeks
early
but is
now
thrivin
g.